Clear Skin With UVb Light Therapy
We treat autoimmune skin conditions and Vitamin D Deficiency with narrowband UVb Light Therapy.
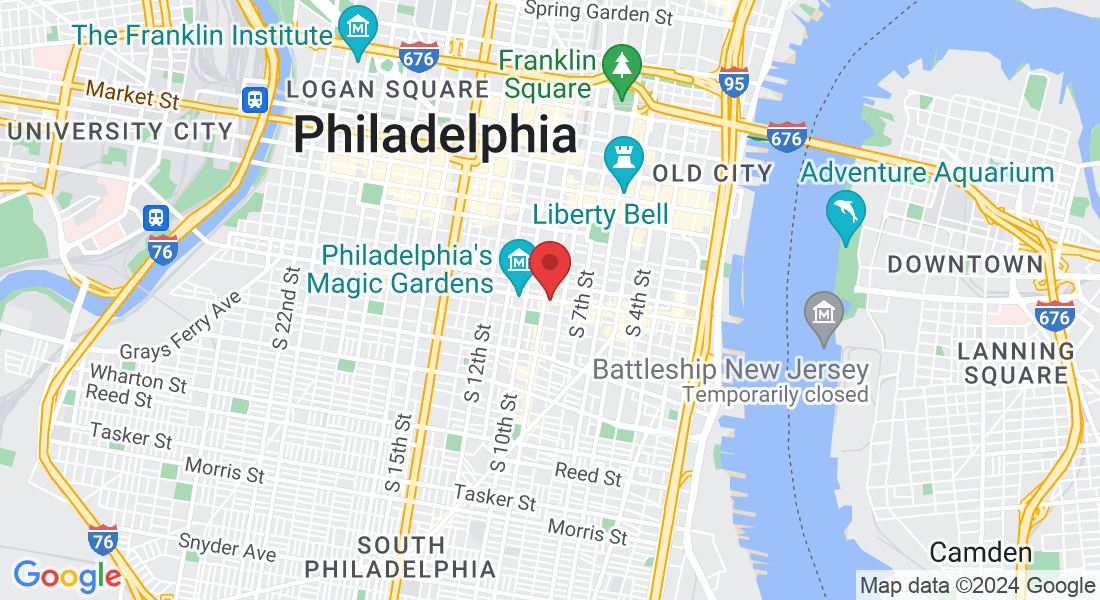
Located in South Philadelphia.
Suffering from a condition like psoriasis, eczema, and vitiligo can feel isolating and overwhelming.
Maybe you avoid wearing short sleeves or shorts in public due to self-consciousness about visible psoriasis patches.
Perhaps you steer clear of swimming pools or beaches to avoid drawing attention to affected skin.
Do you decline invitations to social gatherings or events where skin exposure is expected, fearing judgment or stares.
Maybe it's difficult for you to have intimate relationships or physical contact for fear of rejection or discomfort caused by skin conditions.
Do you find reasons to opt out of activities like sports or exercise classes where skin may become irritated or aggravated, exacerbating psoriasis symptoms.
UV Light Philly offers innovative narrowband UVb light therapy, providing relief and confidence to individuals affected by various skin conditions like psoriasis, eczema and vitiligo, as well as Vitamin D deficiency.
Psoriasis & Eczema
UV light therapy offers effective treatment for psoriasis and eczema, targeting affected areas with controlled exposure to ultraviolet light to reduce inflammation and promote skin healing.
Vitamin D Deficiency
Vitamin D deficiency leads to muscle pain, weak bones, fatigue, weight gain, difficulty sleeping, dizziness, irregular heart beat, poor wound healing, recurring infections and cognitive issues.
Vitiligo
UV light treatment for vitiligo involves exposing the affected skin to ultraviolet light, which stimulates melanocyte activity, leading to repigmentation of depigmented patches and improving the appearance of the skin.
List of Conditions
Dermatitis, Pruritus, Lichen Planus, Pityriasis Rosea, Cutaneous T-cell Lymphoma, Mycosis Fungoides, Granuloma Annulare, Graft-Versus-Host Disease (GVHD), Atopic Dermatitis and more
Why Narrowband UVb Light Therapy?
UV Light Therapy is ideal due to its non-invasive nature, effectiveness in treating various skin conditions, and minimal side effects compared to other treatment options, offering a safe and reliable solution for improved skin health and quality of life.
UV Light Therapy avoids the mess with creams and the untoward side effects of biologics. On average UV Light Therapy is faster and less expensive than other treatment options.
UV Light Therapy is ideal for chronic Vitamin D deficiency that doesn't respond to supplementation.
Plus we have options for you to continue treatment therapy at home.
Why Come To UV Light Philly?
UV Light Philly makes treatment easy and accessible.
UV Light Therapy is a time commitment requiring treatment 2-3x per week.
You shouldn't have to spend more time looking for parking
and waiting for your appointment to start than the actual treatment.
Advanced Equipment
Top of the line and most advanced photo light booth on the market.
Self Scheduling
Schedule yourself to get the dates and times you want up to one month in advance.
Extended Hours
We are open Monday through Friday with weekend hours for your convenience.

Free Parking
We have free parking in our lot at our facility, so you can be in and out as quickly as possible
Referrals Not Required
You do not need a referral to use our light booth, simply start with a consultation with our team.

Insurance Accepted
HSA/FSA funds accepted. Membership plan available.
Medicare and Medicaid
Aetna, Highmark, Tricare, IBX, Health Partners, UHC, Humana, more available upon request
About UV Light Philly

Catie Harris
Nurse Practitioner
Catie is a board certified nurse practitioner with more than 20 years of experience.
Our mission at UV Light Philly is to help you look good and feel good in your skin.
Blog Posts

Understanding Psoriasis Type: Symptoms, Diagnosis, and Best Treatment Options
Understanding Psoriasis Type: Symptoms, Diagnosis, and Best Treatment Options
Identifying your psoriasis type is pivotal in managing the condition. In this guide, we delve into the eight psoriasis types, describe their symptoms, and outline effective treatment methods. Whether it’s plaque, guttate, or the less common erythrodermic psoriasis, you’ll find targeted information here to help you manage your symptoms better.
Key Takeaways
Psoriasis is a complex skin condition with eight types, including plaque psoriasis, guttate psoriasis, inverse psoriasis, pustular psoriasis, and erythrodermic psoriasis. Each type has its own unique symptoms, triggers, and treatment considerations.
Severe forms of psoriasis, such as pustular and erythrodermic psoriasis, can lead to significant health complications and require immediate medical attention. Treatments often include creams, light therapy, medications, and biologics, and are tailored to the type of psoriasis and its severity.
Beyond medical treatment, managing psoriasis effectively requires a holistic approach that includes lifestyle changes, stress management, and support resources to help improve quality of life and manage symptoms comprehensively.
Exploring the Spectrum of Psoriasis Types
Psoriasis is a dermatological condition that’s far from uniform. With eight different types of psoriasis diagnosed, each presents a unique pattern of symptoms, shaped by a combination of genetic and environmental factors. For some individuals, it manifests as scaly patches on the skin, whereas others experience raised, inflamed bumps with scales and lesions. The condition can manifest at any age, with a higher prevalence seen between young adults aged 15-25 and those aged 50-60.
Plaque psoriasis, also known as psoriasis vulgaris, is the most frequently diagnosed form of the condition. This form is identified by its raised, inflamed, red lesions overlaid by a silvery white scale. However, the psoriasis spectrum also includes guttate, inverse, pustular, and erythrodermic psoriasis, each with their unique symptoms and triggers. It’s also not limited to the skin. Some individuals may experience psoriatic arthritis, where the inflammation targets the joints, or nail psoriasis, affecting the nails.
The triggers for psoriasis are just as diverse as its types. From infections and skin injuries to certain medications, numerous factors can spark a flare-up for individuals with a genetic predisposition to the condition. Despite its chronic nature, psoriasis is not a life sentence of discomfort. Various treatment methods exist to manage symptoms, complemented by specific lifestyle practices and coping mechanisms. Some common triggers for psoriasis include:
Infections
Skin injuries
Stress
Certain medications
Cold weather
Smoking
Alcohol consumption
By identifying and avoiding these triggers, individuals with psoriasis can better manage their symptoms and improve their quality of life.
Plaque Psoriasis: The Most Common Form
Plaque psoriasis is the face of psoriasis for many, accounting for the majority symptoms of psoriasis cases. This type is characterized by:
Elevated, red patches on the skin
Covered with silvery scales
Patches can be itchy and cause a burning sensation
Often appearing on the knees, elbows, lower back, and scalp
Although anyone can develop plaque psoriasis, certain risk factors increase the likelihood. These include:
smoking
alcohol consumption
obesity
stress
skin injury
certain medications
a family history of the condition.
Diagnosing this form of psoriasis involves a thorough examination of the skin, scalp, and nails, with a skin biopsy occasionally needed for confirmation.
Guttate Psoriasis: Triggered by Strep Throat
Guttate psoriasis, on the other hand, often appears suddenly and is typically triggered by a streptococcal infection such as strep throat. Manifesting as patchy rash with small, pink-red spots on lighter skin tones and purplish spots on darker skin tones, guttate psoriasis primarily affects specific areas of the entire body only. Other potential triggers include:
viral infections
skin injuries
tonsillitis
stress
Treatment options to treat guttate psoriasis include a variety of options such as:
Steroid creams
Light therapy
Oral medications
Antibiotics (if caused by a bacterial infection)
Diagnosis involves a physical examination of the affected skin, with a skin biopsy sometimes necessary for confirmation.
Inverse Psoriasis: Hidden in Skin Folds
As the name suggests, inverse psoriasis is found in areas of black skin that are typically unaffected by other forms of psoriasis. This type predominantly affects skin folds such as:
the armpits
under the breasts
the genital area
buttocks
other skin folds throughout the body
Unlike other forms of psoriasis, inverse psoriasis is characterized by:
smooth, shiny red lesions without the typical thick, scaly plaques
a distinct appearance that often leads to misdiagnosis, mistaken for conditions like fungal infections or eczema
triggers that include smoking, obesity, certain medications, and infections
A Closer Look at Severe Psoriasis Forms
While most forms of psoriasis primarily cause discomfort, dry skin and cosmetic concerns, some can have severe health implications. These include pustular and erythrodermic psoriasis, both of which demand immediate medical attention.
Pustular psoriasis presents with scaly, discolored patches of skin containing fluid-filled pustules. It can cause systemic symptoms such as fatigue, fever, headache, and tachycardia, and can lead to conditions like conjunctivitis, arthritis, liver damage, and acute renal failure. Triggers for this form of psoriasis include systemic steroid withdrawal, infections, medications, stress, and hypocalcemia.
Erythrodermic psoriasis, on the other hand, is characterized by extensive redness and peeling that affects a significant portion of cracked skin on the body, often 80–90%. This severe form of psoriasis poses a risk to life, with potential complications including the body’s inability to effectively regulate body temperature again. Prompt medical treatment is essential to manage these complications.
Pustular Psoriasis: Beyond the Surface
As indicated by the name, pustular psoriasis is marked by the presence of pus-filled blisters on the skin. These outbreaks can be triggered by a range of factors, such as stress, pregnancy, infections, exposure to UV light, and reactions to medications. Pustular psoriasis is classified into various subtypes, including subacute generalized pustular psoriasis and palmoplantar pustulosis (PPP).
The diagnosis of this rare form of psoriasis involves a comprehensive review of the patient’s medical history, a detailed physical examination, and the specialized knowledge of a dermatologist. While it brings pain and discomfort to the surface, the complications of pustular psoriasis run much deeper, impacting systems beyond the skin.
Erythrodermic Psoriasis: A Rare and Critical Condition
Erythrodermic psoriasis, a rare and potentially life-threatening variant of the condition, requires immediate medical intervention and often hospitalization. The condition is distinguished by:
extensive, red or purple skin with silvery scales
encompassing substantial areas of the body
exfoliation frequently takes place in larger fragments, which differs from the small scales commonly seen in other types of psoriasis.
Treatment for erythrodermic psoriasis may include:
Over-the-counter or prescription corticosteroid creams
Oral medications
Light therapy
Biologics
Additionally, biologics are frequently advised for the treatment of erythrodermic psoriasis.
Despite the potential for severity, with appropriate and timely, medical care and intervention, these critical conditions can be managed effectively.
Psoriatic Arthritis: When Psoriasis Affects Joints
Psoriatic arthritis is another facet of the psoriasis spectrum, affecting between 30% and 33% of individuals with psoriasis. This condition can lead the body and immune system to attack both the joints and skin, typically showing skin symptoms a few weeks before joint symptoms.
Indicative symptoms of psoriatic arthritis encompass:
Swollen fingers and toes
Foot pain
Lower back pain
Inflamed and painful joints (often in the fingers and toes)
Skin rashes
Changes in fingernails and toenails
This painful and physically limiting autoimmune disease is attributed to inflammation in the joints as a result of an overactive immune system, leading to symptoms such as joint pain, stiffness, and swelling.
Nail Psoriasis: More Than Just Cosmetic Concerns
Psoriasis can also affect the nails, causing discoloration, pitting, and in some cases, separation from the nail bed. Nail psoriasis is diagnosed through a physical examination conducted by a healthcare provider, with typical clinical signs including nail pitting, subungual hyperkeratosis, onycholysis, and oil drop discoloration.
Despite being a less common manifestation, the documented frequency of nail psoriasis among individuals with plaque psoriasis treatments ranges from 15% to 86%. While the changes to the nails can cause discomfort and cosmetic concerns, the treatment options for nail psoriasis are comparable to those utilized for plaque psoriasis.
Scalp Psoriasis: Not Just Dandruff
Another variant, scalp psoriasis, causes intense and severe itching, flaking similar to dandruff, and can even lead to temporary hair loss. It is estimated to have an incidence of 45-56% among individuals who have been diagnosed with psoriasis.
This form of psoriasis is not limited to the scalp alone. This condition has the potential to spread from darkened skin on the scalp to areas like the neck, face, and ears. It can appear as one large skin patch or several smaller skin patches.
The treatment options for scalp psoriasis encompass topical treatments, light therapy, oral medications, and biologics.
Identifying Your Type of Psoriasis
Diagnosing psoriasis is a process that combines an examination of clinical features with a comprehensive review of the patient’s medical history. This includes a thorough understanding of past medical conditions and potential triggers or factors that could impact the onset or exacerbation of psoriasis.
In most cases, a skin biopsy is not necessary for diagnosing psoriasis. However, in exceptional instances where the condition presents atypically, a biopsy may be warranted. The findings from a skin biopsy typically do not provide significant new information and are generally reserved for evaluating atypical cases.
Understanding and identifying your type of psoriasis is a critical first step towards effective management. It allows for a targeted treatment plan, paving the way for better symptom control and improved quality of life.
Tailored Treatments for Each Psoriasis Type
When it comes to treating psoriasis, one size does not fit all. Treatment is tailored to the type and severity of the condition, ranging from topical steroids or light therapy to systemic treatments or biologics. In the case of guttate psoriasis, for example, treatment may involve light therapy, exposing the skin to UVA and UVB rays, often in conjunction with prescribed oral medications and ointments to alleviate inflammation.
The treatments for moderate to more severe cases of psoriasis are typically more aggressive. These involve systemic agents and/or phototherapy, aimed at decreasing extensive inflammation and inhibiting the rapid proliferation of skin cells associated with the symptoms of psoriasis. However, it is crucial to be mindful of potential side effects and complications. For instance, the use of systemic corticosteroids is generally avoided due to the risk of triggering a severe form of psoriasis flare-up upon withdrawal.
While medical treatments are vital in psoriasis management, combining them with lifestyle changes and stress management techniques can enhance their effectiveness. A holistic approach to treatment can significantly enhance symptom control, reduce flare-ups, and improve the overall quality of life.
Topical Solutions for Localized Relief
For mild to moderate psoriasis, topical treatments are usually the initial course of therapy. They are typically applied once or twice daily, with the duration of use varying depending on the medication. These treatments can vary based on the type and location of psoriasis. For instance, low-potency steroid creams are used for inverse psoriasis, often combined with antimicrobials.
While topical treatments offer localized relief, they may also lead to potential side effects. These include:
Acne
Skin discoloration
Thinning of the skin
Stretch marks
Easy bruising
Localized hair growth
Burning or stinging sensation upon application
It’s essential to discuss these potential side effects with your healthcare provider to ensure you’re using these treatments safely and effectively.
Systemic Treatment Strategies for Widespread Psoriasis
Systemic treatments are typically required for moderate to very severe cases of psoriasis or psoriatic arthritis. These systemic medications include oral medications and biologics, designed to treat the condition from the inside out. Examples of these biologics include Adalimumab, Etanercept, and Ustekinumab.
While these treatments can be highly effective, they come with their own set of potential side effects. Therefore, biologic therapy should be initiated by specialists who are knowledgeable about these treatments to ensure appropriate management.
It’s also important to note that while oral medications are typically in tablet form, biologics are commonly administered via injections.
Light Therapy: Harnessing UV Rays
UV therapy, especially UVB phototherapy, has demonstrated effectiveness in treating psoriasis. It’s capable of causing skin cells from penetrating the skin and inhibiting the rapid growth of skin cells associated with psoriasis.
UV light therapy, particularly narrowband UVB, is administered through the use of artificial lamps or lasers that emit ultraviolet rays. Despite its effectiveness, it’s crucial to be aware of the potential risks and side effects of light therapy, such as skin damage from overexposure, and to always use it under the guidance of a healthcare professional.
Managing Psoriasis Holistically
A holistic approach to management can offer additional benefits beyond the essential medical treatments for psoriasis. Lifestyle changes such as:
maintaining a healthy weight
incorporating regular exercise
quitting smoking
reducing alcohol consumption
ensuring sufficient sleep
can assist in managing psoriasis.
Stress management also forms an integral part of holistic care for psoriasis. High levels of stress can exacerbate psoriasis symptoms, making stress management techniques such as mindfulness, deep breathing exercises, and seeking mental health support from friends, family, or a therapist crucial components of a comprehensive treatment plan.
Adopting a holistic approach not only helps manage psoriasis symptoms but also addresses the overall well-being of the individual. It’s important to remember that managing psoriasis goes beyond treating the chronic skin condition - it involves caring for the whole person.
Support and Resources
While living with psoriasis can present challenges, remember that you’re not alone. There are numerous resources available to help you navigate your journey with psoriasis. Reputable sources of information and awareness include the National Psoriasis Foundation, Psoriasis.org, and Lilly Medical.
In addition to these resources, online communities such as Psoriasis Association Forums and Psoriasis Club can offer peer support and shared experiences, providing an important sense of community and understanding. Staying updated on the latest developments in psoriasis research other treatments, events, and programs can also be beneficial for those living with the condition.
Summary
Psoriasis is a complex, multi-faceted condition that goes beyond the skin. It presents in various forms, each with unique triggers, symptoms, and treatments. Whether it’s plaque, guttate, inverse, pustular, erythrodermic, psoriatic arthritis, nail, or scalp psoriasis, understanding your type is the first step towards effective management. Treatment options, ranging from topical and systemic therapies to light therapy, along with lifestyle modifications and stress management, can significantly enhance symptom control and improve the overall quality of life. Remember, with the right knowledge, support, and resources, living well with psoriasis is entirely possible.
Frequently Asked Questions
What are the 5 types of psoriasis?
The 5 types of psoriasis are plaque psoriasis, guttate psoriasis, pustular psoriasis, inverse psoriasis, and erythrodermic psoriasis. These types vary in their appearance and severity.
Can you have 3 types of psoriasis?
Yes, it is possible to have more than one type of psoriasis at a time due to the different signs and symptoms of each type of psoriasis. Psoriasis can show up in various ways, such as on the skin, nails, and joints.
What is the most serious psoriasis?
The most serious form of psoriasis is a rare type characterized by red, scaly skin covering most of the body, which can be triggered by factors like severe sunburn or certain medications.
What is the most common subtype of psoriasis?
The most common subtype of psoriasis is plaque psoriasis, which affects up to 80 percent of people with psoriasis. It is characterized by raised, red patches of skin covered by silvery-white scales.
Are there different treatments for each type of psoriasis?
Yes, the treatment for psoriasis is tailored to the type and severity of the condition, with options such as topical treatments, light therapy, systemic treatments, and biologics available.
Look Good, Feel Good In Your Skin
UV Light Philly offers you the ability to leverage the power of light therapy for treatment of autoimmune skin conditions.
Getting Started Is Easy
1. First Time Clients Schedule A Consult
2. Receive Your Treatment Plan
3. Start Self Scheduling Your Therapy
UV Light Therapy Available To You In South Philadelphia.
Get In Touch
Address
Office: 834 South St., Philadelphia PA 19147
Phone Number:
215-709-6149
Email: [email protected]
Hours
Mon – Fri 8:00am – 5:00pm
Sat & Sun – 10:00am - 3:00pm
Referrals
Want To Refer A Client?
Click Here to complete a Referral Form.
We will handle all insurance and billing matters and send you updates on your patient’s light therapy progress.
We ONLY do UV light therapy and send the client back to you for dermatological issues.
Office: 834 South St. Phila, PA 19147
Call 215-709-6149
Email: [email protected]
Site: www.UVLightPhilly.com